What Is Female Urinary Incontinence?
Urinary incontinence is the unintentional passing of urine. It’s a common problem thought to affect millions of people.
There are several types of urinary incontinence, including: stress incontinence – when urine leaks out at times when your bladder is under pressure; for example, when you cough or laugh urge (urgency) incontinence – when urine leaks as you feel a sudden, intense urge to pee, or soon afterwards overflow incontinence (chronic urinary retention) – when you’re unable to fully empty your bladder, which causes frequent leaking total incontinence – when your bladder cannot store any urine at all, which causes you to pass urine constantly or have frequent leaking1. Not to be confused with Urinary Incontinence, Urinary retention is a condition in which you are unable to empty all the urine from your bladder. Urinary retention can be acute—a sudden inability to urinate at all, or chronic—a gradual inability to empty the bladder6.
How Common Is Urinary Incontinence?
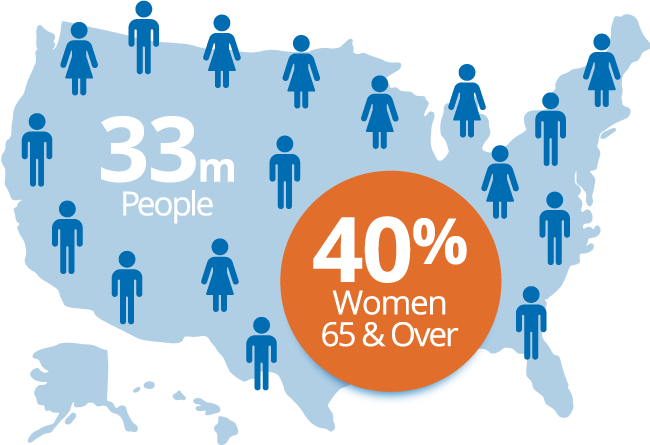
As many as 3.3 million Canadians — nearly 10% of the population — experience some form of urinary incontinence2. Urinary incontinence is more common in women than in men—in fact, it affects more than twice as many women than men.
The prevalence also increases with age, making it more common in older females; about 40% of women aged 65 and older have some form of urinary incontinence3.
Types of Urinary Incontinence
The most common types of urinary incontinence in women are:
Stress incontinence
The most common type of urinary incontinence, stress incontinence happens when an action puts pressure on the bladder, causing urine leakage. Coughing, sneezing, jogging or exercising, lifting something heavy, and even laughing can contribute to urine leaks3.
Urge incontinence
Sometimes called “overactive bladder,” urge incontinence occurs when you experience a sudden, strong urge to urinate, followed by urine leakage you can’t control. You may feel the need to urinate often or when you don’t expect it, including throughout the night, during sleep or after drinking water. This type of urinary incontinence is more common in older women3.
There is also functional incontinence. With this type of incontinence, a disability or obstacle keeps you from making it to the restroom in time. For example, you may have trouble walking and can’t get to the restroom in time, or you have arthritis in your hands that makes it difficult to undress before you begin to urinate4.
What Causes Urinary Incontinence?
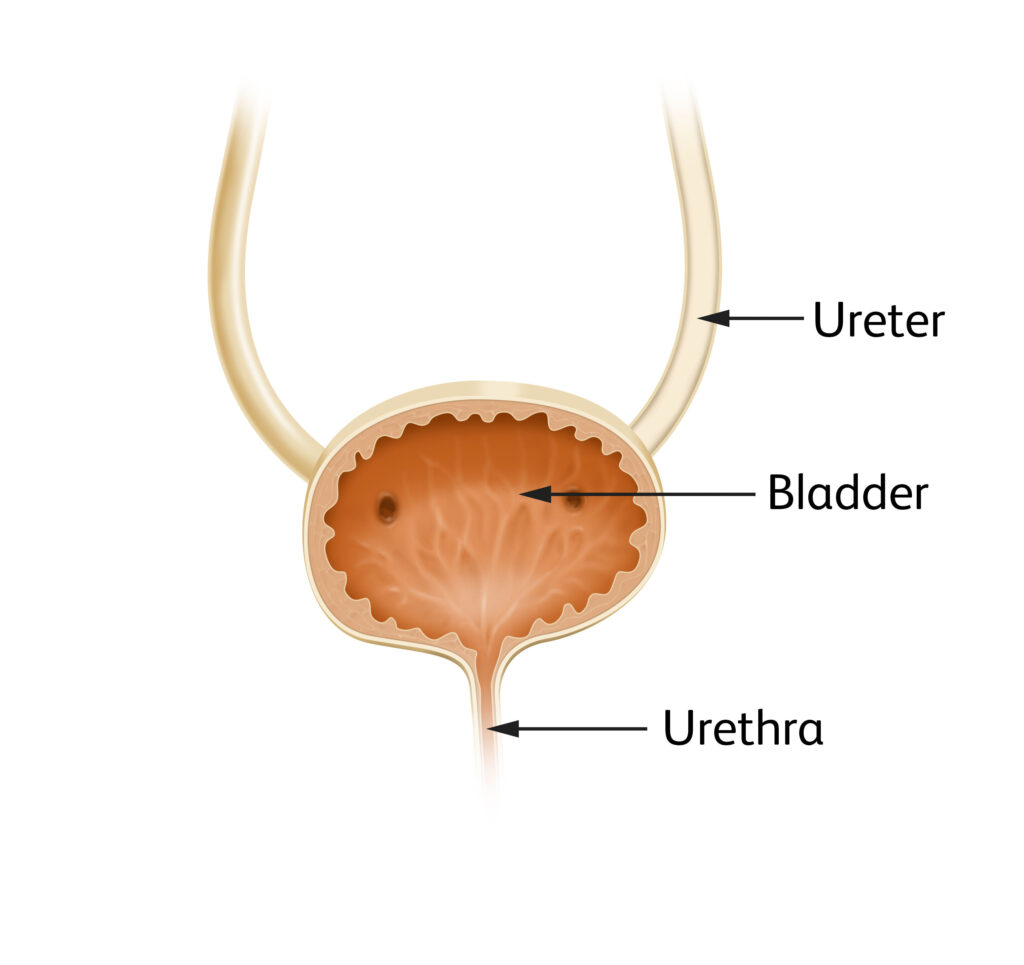
Urinary incontinence is usually caused by problems with the muscles and nerves that help the bladder hold or pass urine5.
Urinary incontinence is not a disease; rather, it is a symptom of a wide range of health issues that can be both temporary or prolonged:
Temporary incontinence includes urinary tract infections (UTI), certain medications, and constipation. In cases like these, the incontinence lasts a short time4. Additionally about one-third of women have urinary incontinence (UI) after childbirth7.
Long-term (chronic) incontinence can be the result of an underlying condition (such as a neurological disorder) or a change or event the body goes through, such as menopause or a hysterectomy4.

Causes In Men vs Women
The temporary causes mentioned above can often apply to both men and women.
Although urinary incontinence in women can happen at any age, it’s more common in older women; in fact, about 4 in 10 women aged 65 and older have female urinary incontinence. Researchers believe that the low levels of estrogen after menopause may weaken the urethra, which keeps urine in the bladder until you are ready to urinate. In men, incontinence is often related to prostate problems or treatments3.
Treatment Options for Urinary Incontinence
Although the incidence of urinary incontinence increases with age, despite what many people think, it’s not necessarily a normal condition that you simply must learn to live with. Urinary incontinence can be treated, and the first step to doing so is having an honest discussion with your doctor. It is important to understand that there are behaviour, pharmaceutical, and surgical options available as possible treatment methods7.

Discussing Urinary Incontinence With Your Doctor
Because the treatment or management for urinary incontinence will vary with each individual, it’s important to discuss your symptoms with your doctor.
It’s not uncommon to be hesitant or even embarrassed to talk about bladder problems in women with a doctor. A little preparation can help your appointment be productive, and these tips can help you to discuss your incontinence with your doctor:

Track your symptoms.
Record your symptoms for several days to help your doctor better understand patterns, times, and causes of your urine leakage.

Write down questions.
It can be frustrating to leave the doctor and realize you forgot to ask her something. Writing down your questions can help ensure all of your concerns can be addressed.

Bring a list of your medications.
This includes any supplements, vitamins, or OTC medications as well as prescriptions. Its important to be open about this to your doctor to ensure any new medications he prescribes do not react with something you’re currently taking.

Do a little research.
Learn more about the various treatment options for urinary incontinence and ask your doctor about the ones you’re interested in, or ones you think would be helpful.

Bring an advocate.
Some people find it helpful to bring a trusted advocate, such as a partner, caregiver, or family member, to their appointments with them.
You can begin your discussions about female incontinence with your primary care doctor or OBGYN. Your provider may also refer you to a specialist if they decide you need a different treatment or additional diagnosis. These specialists are usually urologists, who specialize in urinary issues in men and women, or a urogynecologist, who specializes in the female urinary system.
Managing Urinary Incontinence At Home
There are things you can do to manage your urinary incontinence at home as well. Some people with urinary incontinence find the following tips helpful for managing urine leakage in women:
- Kegel/pelvic floor exercises. These exercises may help strengthen your pelvic floor muscles.
- Lose weight, if needed. If you’re overweight, losing weight can help reduce the pressure that excess weight puts on your bladder and surrounding muscles.
- Quit smoking. Smoking can exacerbate urinary incontinence.
- Reduce caffeine and alcohol consumption. Alcohol and caffeinated beverages are diuretics, which stimulate the bladder and increase urine volume.


Urinary Incontinence and Sleep
Urinary incontinence can also affect your sleep. Not only does waking throughout the night to use the bathroom disrupt your sleep schedule, urine leakage or bedwetting can result in disrupted sleep as well.8
If you urinary incontinence is affecting your ability to get a good night’s sleep, a trip to the doctor may be in order. In the meantime, these tips may help you avoid accidents at night:
- Limit fluid intake before bedtime. This is especially true for alcohol and caffeinated beverages, as mentioned above.
- Try to double-void before bed. Urinate twice before you go to bed—once when you begin your nighttime routine and once again right before you lie down for the night
- Consider products to help manage leaks. There are also products that may help manage urine leakage and reduce bedwetting incidents. These include pads, liners, or a nighttime urine collection system like the PureWick™ System.
Finding Support for Urinary Incontinence
The most important thing to remember is that you don’t have to manage your urinary incontinence alone. Working with your healthcare provider, learning more about urinary incontinence, and finding the right products can help you manage your condition.
Sources:
- NHS. (n.d.). Urinary incontinence. NHS choices.
- Diagnosis, treatment & symptoms of urinary & bowel incontinence. The Canadian Continence Foundation. (n.d.).
- Urinary incontinence. Urinary incontinence | Office on Women’s Health. (n.d.). https://www.womenshealth.gov/a-z-topics/urinary-incontinence
- Mayo Foundation for Medical Education and Research. (2023, February 9). Urinary incontinence. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/urinary-incontinence/symptoms-causes/syc-20352808
- How does the urinary system work? – informedhealth.org – NCBI bookshelf. (n.d.). https://www.ncbi.nlm.nih.gov/books/NBK279384/
- U.S. Department of Health and Human Services. (n.d.). Definition & Facts of urinary retention – NIDDK. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/urologic-diseases/urinary-retention/definition-facts
- Gibbs et al, Office management of geriatric urinary incontinence, Am J Med, 2007;120(3):211-20
- Welk, B., & Kennelly, M. (2022). The relative importance of different consequences of nocturnal enuresis among older women: A conjoint analysis experiment. Neurourology and Urodynamics, 41(6), 1451–1457. https://doi.org/10.1002/nau.24980